The first signs of cervical osteochondrosis are quite difficult to recognize. Often they cause so little discomfort that a person does not pay attention to them and is in no hurry to see a doctor. In other cases, the symptoms are confused with simple fatigue or a mild cold:
- increasing pain in the neck;
- feeling of heaviness in the back of the head;
- slight tingling in the hands.
These signs occur in thousands of people every day, but few can recognize them as developing cervical osteochondrosis.
Important! Remember that the disease develops slowly and in the initial stages it is much easier to curb the progression of destructive processes than to treat an advanced stage!
Who is at risk?
Osteochondrosis develops not only in people who lead a sedentary lifestyle. Athletes from areas such as classical wrestling, judo, freestyle wrestling and sambo also suffer from this disease. The disease arises from critical loads on the spine in the neck area (constant falls and blows, high mobility of the neck). It is important to remember that osteochondrosis is often diagnosed before the age of 35 - in over 86% of cases.
How the disease develops
Currently, osteochondrosis of the cervical spine is much more common than other diseases of the spine. This is due to the greater mobility of the neck. As the disease progresses, severe pain appears, making a person's life worse. Osteochondrosis progresses slowly, but certainly leads to degenerative changes in the bone tissue of the spine. There are four degrees of development of the disease:
- The first stage is characterized by an almost complete absence of symptoms. The disease can only be diagnosed during a routine examination. Mild pain may sometimes occur, which many consider to be a sign of stress or fatigue. In the first stage, the nucleus pulposus is destroyed, as a result of which the vertebrae begin to bear the load more poorly. As a result, degenerative-dystrophic processes develop. The first symptoms include: mild headaches that quickly disappear, a cramp syndrome "in the neck" and severe muscle tension in the upper back.
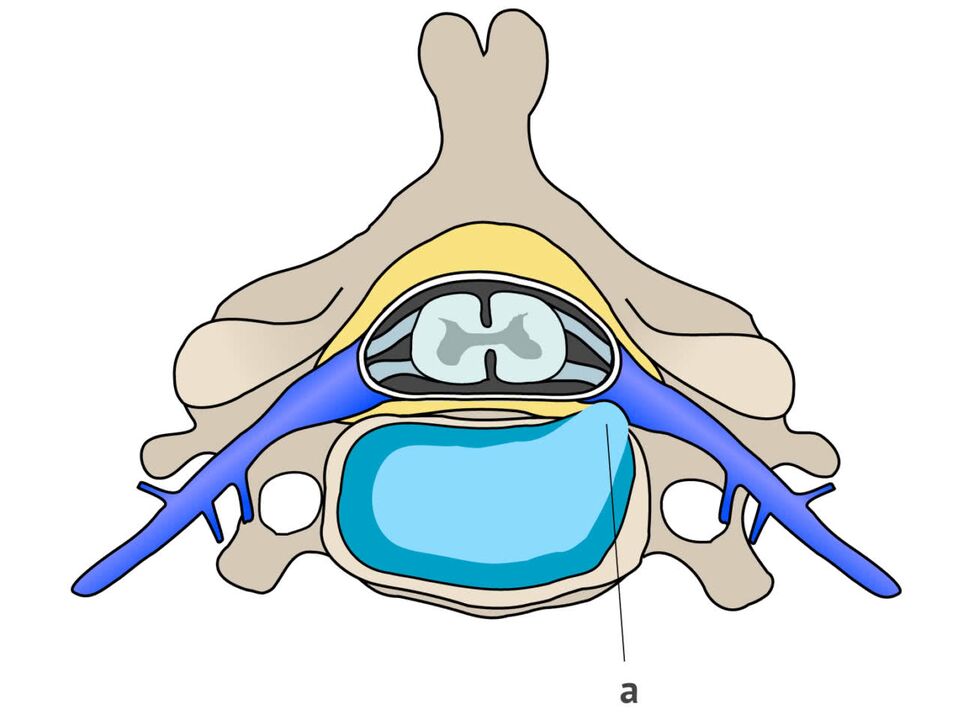
- In the second stage of the disease, cracks appear on the sides of the intervertebral discs due to stress. They are not very deep yet, but are already helping to push the core out. During diagnosis, a protrusion is often noted and the height of the intervertebral disc decreases. This stage is characterized by frequent and persistent pain. A person loses strength, certain areas of his face begin to go numb, and stiffness of movements develops due to fear of new pain sensations.
- The third stage is characterized by the formation of a hernia in the neck area between the vertebrae. All tissues and the vessels in this area are also affected - veins, muscles, nerves, arteries. The pain flows gently and spreads from the neck to the back of the head. When you move your head, a special sensitivity arises. Patients also complain of dizziness due to insufficient blood flow to the vertebral artery.
- In the fourth stage, osteophytes form - the bone tissue becomes wider because the body and brain literally send signals that require an increase in area to distribute the load. This pinches the nerves of the vertebrae, reduces the size of the cavities between the vertebrae, causes severe stiffness and sometimes inability to move. All adjacent joints are damaged. To eliminate the causes and "contain" cervical osteochondrosis at this stage, long-term and difficult treatment, including surgical intervention, is required.
Preventing cervical osteochondrosis is an important process that helps curb the breakdown of the cervical vertebrae, alleviate complications, and preserve your quality of life. However, to detect pathology, you need not only to monitor the symptoms, but also to diagnose and take the necessary tests at least once a year.
Features of symptoms of cervical osteochondrosis
Even minor changes to the vertebrae, ligaments and intervertebral discs lead to dysfunction of the nerve endings. Blood vessels are also affected. All of them are directly connected to the brain and other organs, causing unpleasant symptoms.
Important! It is the compression of blood vessels and nerves that causes discomfort and severe pain.
Clinical symptoms of cervical osteochondrosis are divided into three groups:
- The first group is characterized by neurological manifestations of pathology arising from the impact of inflammatory processes and changes in tissues on the peripheral part of the nervous system.
- the second group is associated with the impact of processes on the spinal cord;
- The third group includes signs based on disruption of processes in the nerve endings leading to the brain.
As soon as disorders occur in the peripheral nervous system, people begin to feel pain. They don't always start abruptly and last for a long time, but they all start in the same place - in the neck. The pain is not similar to muscle pain and there is no relaxation when kneading.
In most cases, damage to the peripheral system results in a feeling of shortness of breath. Patients feel like they have a lump in their throat and find it difficult to breathe. The pain is characterized by the fact that it is unspoken, dull and constant tension is felt in the muscles. Sometimes the pain increases after a night's sleep.
As the disease progresses, symptoms spread. After the head and neck, the arms begin to suffer:
- feel weak;
- Numbness occurs in one or more fingers;
- then large parts of the hands become numb.
If you feel pain and pressure in the heart area, you can talk about the development of cervicothoracic osteochondrosis. Osteochondrosis is often misidentified as angina or neuralgia. It is mainly characterized by symptoms such as:
- Cough;
- Stomach pain;
- liver problems;
- Pain in the lungs.
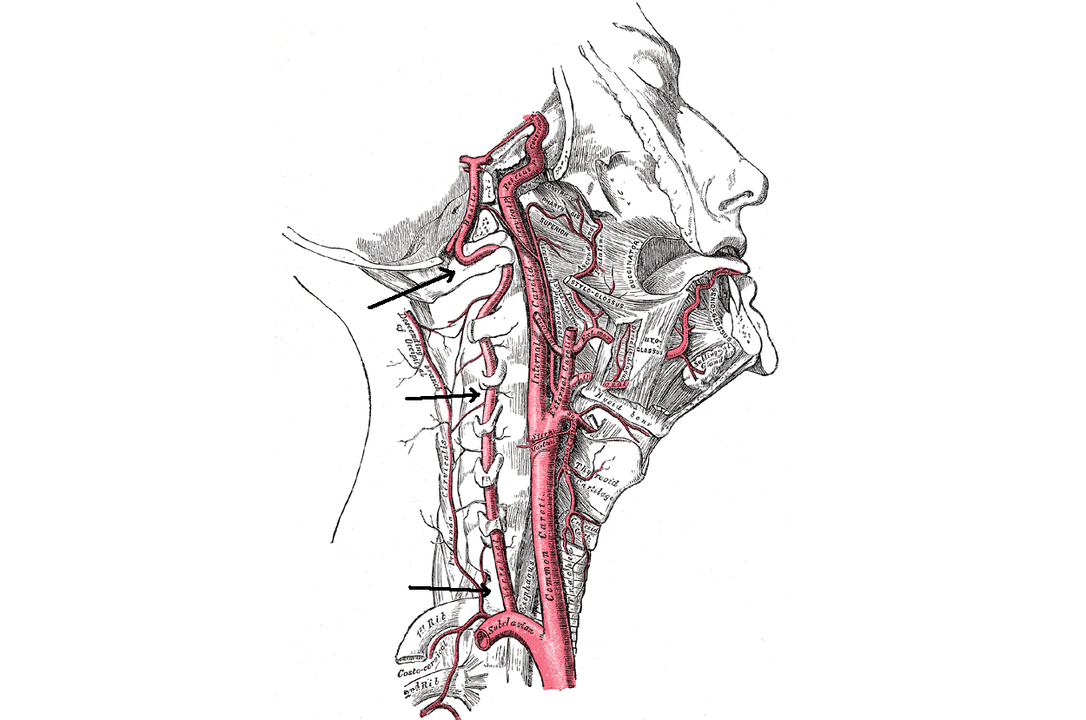
Once the vertebral artery is connected to the destructive process (it supplies oxygen to the brain), symptoms appear from the brain. As the disease develops, it becomes trapped and can no longer function normally. This causes dizziness, blurred vision and tinnitus.
The use of conventional painkillers rarely helps with headaches associated with cervical osteochondrosis.
Physical activity and frequent nervous stress can provoke an exacerbation of the pathology. Symptoms of exacerbation of cervical osteochondrosis:
- increasing irritation;
- sensitive and intermittent sleep;
- rapid fatigability.
When a person is diagnosed with vegetative-vascular dystonia, the symptoms intensify: neuroses develop, blood pressure rises. The diagnosis may also indicate the development of cervical osteochondrosis. Therefore, it is necessary to pass all the tests, undergo an MRI and take additional images of the cervical spine.
It is almost impossible to independently diagnose cervical osteochondrosis based on symptoms. Since the first stage proceeds with practically no obvious signs, it is necessary to undergo regular preventive examinations. At the first signs of the disease, treatment should be started according to the doctor's recommendations. Even if the disease has not yet "played out" and is not causing any noticeable problems.
Syndromes
For an accurate diagnosis of cervical osteochondrosis, correct justification of the symptoms is necessary. The doctor must use tests, images and examinations to accurately determine the causes of the symptoms. They are all associated with certain syndromes.
Humeroscapular periarthritis
The syndrome is characterized by severe pain and muscle contractures in the area of one of the shoulder joints. In left-handed people, the left shoulder joint is usually affected; in right-handed people, the right shoulder joint is affected. Features of pain syndrome:
- Constant;
- Pain;
- Pain.
In most cases, the pain worsens at night. Moving your hand to the side or placing it behind your back also increases the pain. Sometimes pain can be felt throughout the arm, the back of the head and the shoulder blade area.
During the examination, the doctor often notices tension in the joint area and when palpating the patient feels severe pain in the muscles. In some cases, the doctor finds densities and small nodules during palpation and there is slight swelling of the affected shoulder.
Radicular syndromes
The syndrome can occur when the spinal root is damaged. It usually occurs several years after the onset of osteochondrosis. Irreversible destruction occurs in the vertebrae and intervertebral discs: the cavity consisting of nerves and vessels becomes smaller as the cartilage becomes thinner or an intervertebral fracture forms. Osteochondrosis with radicular syndrome is characterized by certain symptoms:
- Pain is observed in the forearm, in the scapula area and moves to the front of the chest;
- it becomes difficult to move the neck, pain and stiffness are felt;
- The sensitivity of the skin on the hands worsens, it becomes numb and a feeling of "goosebumps" appears.
- A person cannot lift his hand from the side of the affected parts.
Irritable reflex syndrome
The syndrome is characterized by a mild burning, stabbing pain in the back of the head and neck. It occurs when you move your head after a long period of immobility, such as while working at a computer. There are complaints in the shoulder joints and in the chest area.
cardiac syndrome
The syndrome is often confused with angina pectoris because the symptoms of the diseases are almost identical. This happens because the compression of the roots in the lower sections of the cervical spine causes pain and contractions of the muscle tissue in the area of the heart. Hence the similarity of the diseases.
The syndrome is characterized by pain that occurs in episodes and can last between 10 and 15 minutes to several hours. Become significantly stronger with sudden movements (spinning, coughing, sneezing). Cardinal syndrome is often characterized by the development of tachycardia, and coronary dilators cannot relieve the pain. The cardiogram also shows no signs that are characteristic of circulatory disorders.
Vertebral artery syndrome
The job of the vertebral artery is to supply the brain and spinal cord. In the syndrome, the work of the periarterial sympathetic plexus is disrupted. The syndrome picture looks like this:
- headaches of varying intensity;
- Disturbances of the vestibular system (swaying, loss of balance);
- mild and severe dizziness;
- nausea, vomiting;
- Throat and eye symptoms (deterioration in vision, appearance of a haze in front of the eyes).
With vertebral artery syndrome, burning pain often occurs not only in the neck but also in the back of the head. A feeling of lethargy, resentment and irritability develops. Anxiety levels increase, sleep and memory may be disturbed.
Therefore, in order to make an accurate diagnosis, it is necessary to determine which syndrome is the basis of cervical osteochondrosis. Based on specific symptoms, test results, photos and palpation, an experienced doctor can accurately determine the features of the pathology and prescribe the correct treatment.





















